Healthcare Revenue Cycle Management Services
Accelerate 40% cash flow, decrease denials, increase & speed-up net collections, reduce days in A/R, enhance the patient experience, and reduce bad debt with Bolster’s Revenue Cycle Management Services with 20+ years of billing and coding expertise and experience.
What revenue cycle management success looks like
So many of our clients have seen…
500+ Healthcare Professionals &
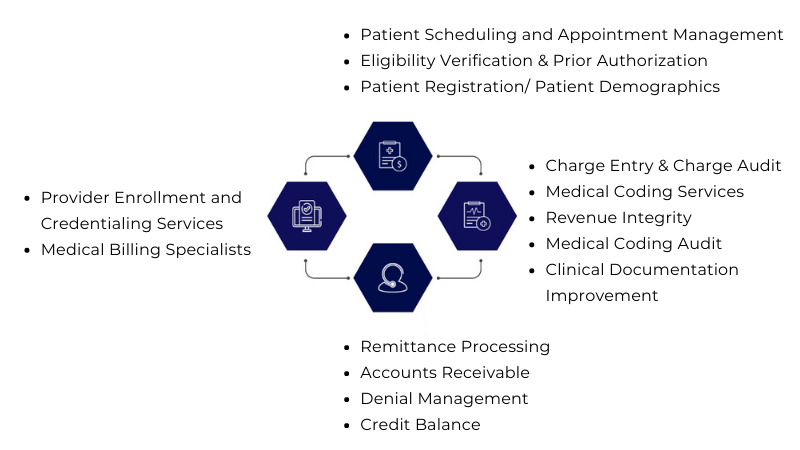
200+ Hospitals have benefitted from our :
At Bolster, we dive deeper into eEligibility so you will know exactly what to expect for that patient and their relationship with the insurance provider.
Bolster RCM department has a significant rapport with most insurance companies, drastically speeding up the process for any new enrollment for existing providers or if you are adding a provider.
We employ highly experienced, AHIMA-credentialed coders for medical coding support and auditing services.
We create customized reports with advanced tools to measure business performance.
At Bolster, we work to prevent future delayed payments so your practice receives payment sooner and more often.
Bolster RCM is adept at working with multiple practice management software systems. So, when your practice comes on board we can work to help reduce your outstanding A/R.
We track each insurance company's timeline and report the status of the claims. We can even track differences by state.
Our team vigorously follows up with insurance to collect money and for patient collections, we sends out two statements to the patient and Either through inbound or outbound follows up with a phone call to make sure you get paid, all while letting you focus on managing the practice.
Getting started with RCM services
Achieving dramatic business growth is as easy as 1, 2, 3…
Tell us your financial and operational goals, get your questions answered, and discover how much our team can increase your revenue and efficiency.
Our proven process has increased our clients’ revenue typically by 40% -50% and sometimes even more. Together, we'll build a perfect plan for you.
You’ll see increased revenue, have more money in the bank, and operate more efficiently. In fact, our 30-day guarantee guarantees it!
How much does our RCM services cost?
BolsterRCM cost generally ranges from 3% to 6% based on the collection amount.
However, your fee can actually be 0% when factoring in how:
- 🎯 our financial/management platform and cloud hosting are included as part of our service helping to consolidate your medical services technology spend
- 🎯 our team of 30+ billing and EDI experts reduces your in-house staffing and operational costs
- 🎯 we’ll increase your revenue – guaranteed – over whatever healthcare revenue cycle management company or in-house system you’re currently using
The sum total on the points above = more income to your practice than our fee!
Revenue Cycle Management - FAQs
We know selecting a revenue cycle management services company can be difficult. You probably have loads of questions, so let’s get you started on some of the most frequently asked questions we get.
How long does it take to transition to your healthcare RCM service?
We can start to submit your claims in as little as 30 days once our 5-7 days of testing is completed.
Will I have single or multiple points of contact with your RCM service?
A BolsterRCM Services Manager, experienced in your specialty(ies), is assigned under which the following resources operate:
- Dedicated Account Manager
- Billing Team Members
- EDI specialists for claims, remittances, EOB reconciliations, eligibility verifications, and direct fund deposits
- HL-7 interface specialist
- A senior member of the ADS management team is also connected with each BolsterRCM client
How will my current databases be handled?
We import your current files such as Referring Physician, Insurance, and Fees into our practice management system.
Does your healthcare RCM service start sending our claims from Day One?
No one wants to submit all of your claims more than we do since we only get paid on amounts collected. But, that would be irresponsible. Instead, we submit test claims for 50 to 100 of your patients for approximately 5 to 7 days. All of your claims are submitted once the test claims are verified.
What happens if my current RCM company stops submitting our claims?
We can bill and resubmit claims from your current medical revenue services team to expedite patient payments. In fact, BolsterRCM tracks old claims vs. new claims.
What if we need customized management reports?
Healthcare providers almost never need truly customized reports since our reports/dashboards as so highly user-defined and are exportable to Excel. But if a certain customized report(s) are needed, your Accounts Team will provide the same via standard PDF or Excel.
Are forms needed for electronic claims?
Possibly, and if so, we provide you with whatever form(s) are needed by any insurance payer(s) and provide assistance, if needed, in completing them. Of course 100% electronic claims and EOB reconciliations – which our team handles for you – are encouraged.
30 Days to a Healthier Revenue Stream, Guaranteed!
Fill out the form below to get a customized quote.



